Background
Allogeneic hematopoietic stem cell transplants (allo-SCT) are potentially life-saving interventions used to treat hematologic disorders. Recent studies have shown that living in rural areas may predict worse outcomes after allo-SCT. Marginalization, a term that encompasses social and health-related factors affecting individuals, is predictive of adverse health outcomes. The Ontario Marginalization Index (ON-Marg), an administrative index using variables obtained from census data, was used to identify marginalization status (quintile 1-least marginalized; quintile 5-most marginalized) encompassing four domains: residential instability (area-level concentrations of people who experience high rates of family or housing instability), material deprivation (area-level concentrations of inability for individuals and communities to access and attain basic material needs), dependency (area-level concentrations of people who do not have income from employment), and ethnic concentration (area-level concentrations of people who are recent immigrants and/or a visible minority). In a publicly-funded healthcare context, it is important to know how marginalization impacts survival for patients undergoing allo-SCT.
Methods
We performed a retrospective population-based study using administrative healthcare databases from Ontario, Canada. Patients were included if they were 18 years or older at the time of allo-SCT, and had undergone allo-SCT for acute myeloid leukemia (AML), myelodysplastic syndrome (MDS) or acute lymphoblastic leukemia (ALL) between 2010 and 2022. Patients were excluded if they were a non-Ontario resident at the time of allo-SCT and as a result lacked ON-Marg data. Patients who received allo-SCT for a different indication were excluded.
The primary outcome of this study was 2-year overall survival (OS) from time of transplant to death or end of the study period, based on ON-Marg quintiles. Multivariable Cox regression analysis was used to identify baseline characteristics associated with OS, with ON-Marg as the main exposure.
Results
A total of 1961 patients underwent allo-SCT for AML/MDS/ALL. The median age of patients undergoing allo-SCT was 55 years (IQR 43-63), and 55% of patients were male. 40% of patients had high aggregated diagnosis group (ADG) comorbidity burden, and a majority of patients (64%) lived within 50 kilometers (km) from the transplant center, with a mean distance of 33 km in the entire study population. The distribution of patients across each quintile of marginalization was not always uniform. For ethnic concentration, 24% of patients were in quintile 5, with 17% of patients in quintile 1. For dependency, 19% of patients were in quintile 5, and 25% of patients were in quintile 1.
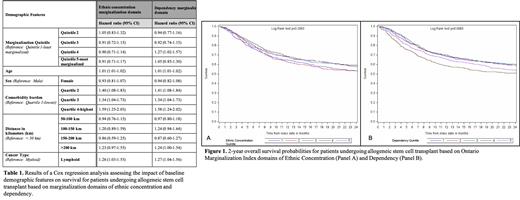
During the follow-up period, 43% of patients (n = 842) died. 2-year OS was not significantly different across all quintiles of the ethnic concentration domain of marginalization ( Figure 1A). 2-year OS was worse (HR 1.27, 95% CI 1.02-1.57) for patients in quintile 4 compared to quintile 1 of the dependency domain of marginalization ( Figure 1B). This effect persisted in multivariable logistic regression analyses accounting for other demographic variables ( Table 1). Increased age and a higher comorbidity index were significantly associated with worse survival across all domains. Patients with ALL had worse outcomes compared to patients with AML/MDS across all domains of marginalization. There was also a trend toward patients living >200 km from the transplant center having an increased risk of death compared to patients living less than 50 km from the center (HR 1.24, 95% CI 1.00-1.54).
Conclusion
This study shows that 2-year OS after allo-SCT for AML/MDS/ALL was not affected by marginalization quintile of ethnic concentration. This is in keeping with other published data suggesting that outcomes after allo-SCT are not impacted by socioeconomic factors such as race. Patients in quintile 4 of dependency had worse outcomes than patients in quintile 1, suggesting that employment and income support are crucial to successful patient outcomes. A majority of patients who underwent allo-SCT lived in close proximity to the transplant center. Transplant outcomes in general do not appear to vary based on marginalization status, and it is therefore crucial that all patients who may benefit receive allo-SCT regardless of demographics or distance to treatment centers.
Disclosures
Prica:Astra-Zeneca: Honoraria; Kite-Gilead: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal